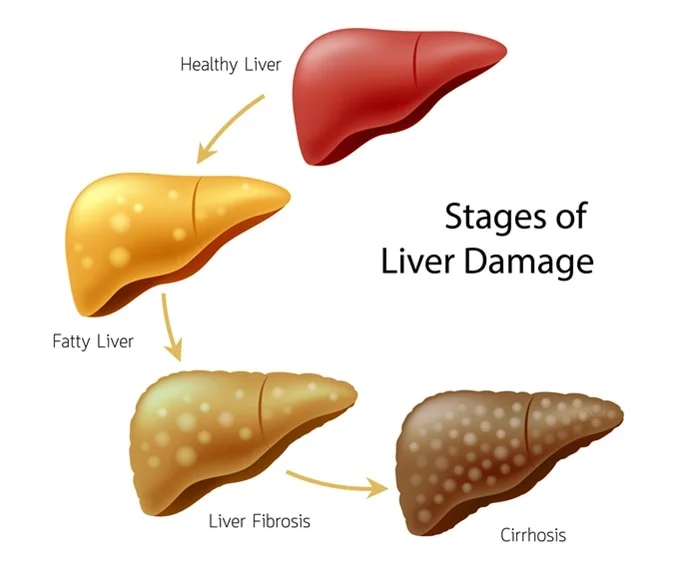
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. Each time your liver is injured, it tries to repair itself. In the process, scar tissue forms. As the cirrhosis progresses, more and more scar tissue forms, making it difficult for the liver to function.
Symptoms:
The symptoms of cirrhosis can vary depending on the severity of liver damage. Some common symptoms include:
- Fatigue and weakness
- Easy bruising and bleeding
- Swelling in the abdomen (ascites) and legs
- Itchy skin
- Yellowing of the skin and eyes (jaundice)
- Poor appetite and weight loss
- Confusion and difficulty concentrating
- Red palms
- Spider-like blood vessels on the skin
Causes:
- Alcohol-related liver disease: Chronic alcohol abuse can lead to cirrhosis.
- Chronic viral hepatitis: Infections with hepatitis B, C, and D can cause cirrhosis.
- Nonalcoholic fatty liver disease (NAFLD): Accumulation of fat in the liver, often associated with obesity and metabolic syndrome.
- Iron buildup in the body (hemochromatosis): A genetic disorder that causes the body to absorb and store too much iron.
- Cystic fibrosis: A genetic disorder that affects the lungs and digestive system, causing the production of thick and sticky mucus that can block the bile ducts in the liver.
- Bile duct disorders: Diseases such as primary biliary cirrhosis, primary sclerosing cholangitis, and biliary atresia can lead to cirrhosis.
- Genetic digestive disorder: Diseases such as Alagille syndrome and Wilson’s disease.
- Liver disease caused by your body’s immune system (autoimmune hepatitis): The immune system attacks liver cells, leading to inflammation and cirrhosis.
Treatment:
The treatment of cirrhosis depends on the underlying cause and the extent of liver damage. Common approaches include:
- Treating the underlying cause: For example, antiviral medications for hepatitis, alcohol cessation for alcohol-related cirrhosis, and weight loss for NAFLD.
- Symptomatic relief: Medications may be prescribed to manage symptoms such as itching, fatigue, and fluid retention.
- Liver transplant: In severe cases where the liver is significantly damaged, a liver transplant may be considered.
- Complication management: Treatment to manage complications like portal hypertension, ascites, and hepatic encephalopathy.
Prevention:
- Limit alcohol intake: Excessive alcohol consumption is a major cause of cirrhosis. Moderation or abstinence is recommended.
- Vaccination: Get vaccinated against hepatitis A and B.
- Maintain a healthy weight: Avoid obesity and manage conditions like diabetes that can contribute to fatty liver disease.
- Practice safe sex: Hepatitis B and C can be transmitted sexually, so practicing safe sex can reduce the risk.
- Avoid sharing personal items: Avoid sharing needles, razors, or toothbrushes, as this can reduce the risk of viral hepatitis transmission.
- Regular medical check-ups: Early detection and management of liver diseases can prevent the progression to cirrhosis.