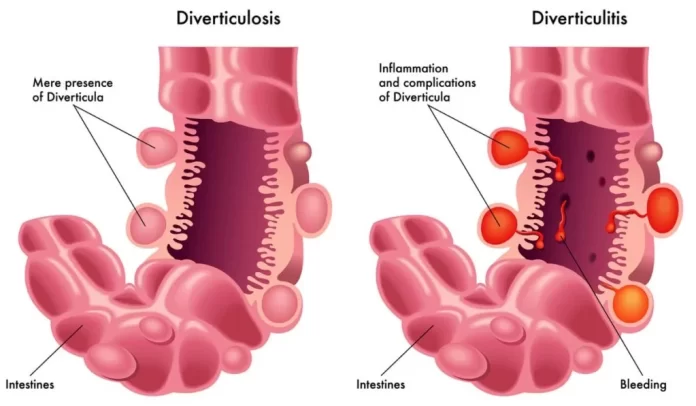
Diverticular disease refers to a condition characterized by the presence of small pouches, called diverticula, that protrude outward from the colon wall. These pouches typically develop in weak spots of the colon where blood vessels penetrate the muscle layer, forming small herniations. The condition is more common in older adults and is associated with factors such as a low-fiber diet, obesity, lack of exercise, and smoking.
There are two main stages of diverticular disease:
- Diverticulosis: This is the presence of diverticula without inflammation or other symptoms. Many people with diverticulosis remain asymptomatic and may not even be aware they have the condition unless it is discovered incidentally during a diagnostic procedure such as a colonoscopy.
- Diverticulitis: This occurs when the diverticula become inflamed or infected. Symptoms of diverticulitis may include abdominal pain (typically in the lower left side), fever, nausea, vomiting, constipation, or diarrhea. Complications of diverticulitis can include abscess formation, perforation of the colon, or even more severe conditions like peritonitis.
Symptoms:
Diverticulosis (without inflammation):
- Often asymptomatic (no symptoms)
- Some individuals may experience mild symptoms such as bloating, cramping, or changes in bowel habits.
Diverticulitis (inflamed or infected diverticula):
- Abdominal pain, usually in the lower left side, that may be severe and persistent
- Fever
- Nausea and vomiting
- Changes in bowel habits, including constipation or diarrhea
- Rectal bleeding (less common)
Causes:
- Low-fiber diet: Lack of dietary fiber can lead to constipation and increased pressure in the colon, contributing to the formation of diverticula.
- Age: Diverticular disease is more common in older adults.
- Obesity: Excess weight can increase pressure within the colon.
- Lack of exercise: Sedentary lifestyle can contribute to constipation and decreased colon motility.
- Smoking: Smoking has been associated with an increased risk of developing diverticular disease.
Treatment:
Diverticulosis (without inflammation):
- Dietary changes: Increasing fiber intake through fruits, vegetables, and whole grains to promote regular bowel movements and prevent constipation.
- Symptomatic treatment: Over-the-counter medications may help alleviate mild symptoms such as bloating or cramping.
Diverticulitis (inflamed or infected diverticula):
- Antibiotics: Prescribed to treat the infection.
- Clear liquid diet: Initially to rest the bowel and gradually reintroduce solid foods as tolerated.
- Pain management: Over-the-counter or prescription pain medications may be needed to manage abdominal pain.
- Hospitalization: Severe cases or complications such as abscess formation may require hospitalization and intravenous antibiotics.
Surgery: Reserved for complicated cases or recurrent diverticulitis that doesn’t respond to medical treatment. Surgery may involve removing the affected portion of the colon (colectomy).
Prevention:
- Dietary changes: Consuming a high-fiber diet rich in fruits, vegetables, and whole grains to promote regular bowel movements and prevent constipation.
- Regular exercise: Engaging in regular physical activity to maintain overall colon health and prevent constipation.
- Maintaining a healthy weight: Avoiding obesity and excess weight, which can increase pressure within the colon.
- Avoiding smoking: Quitting smoking, as it is associated with an increased risk of diverticular disease.
- Hydration: Drinking plenty of fluids to maintain adequate hydration and soften stools, reducing the risk of constipation.
It’s important for individuals with diverticular disease to work closely with their healthcare providers to develop a personalized treatment plan and make necessary lifestyle modifications to manage the condition effectively. Regular medical follow-ups are also essential for monitoring the condition and preventing complications.