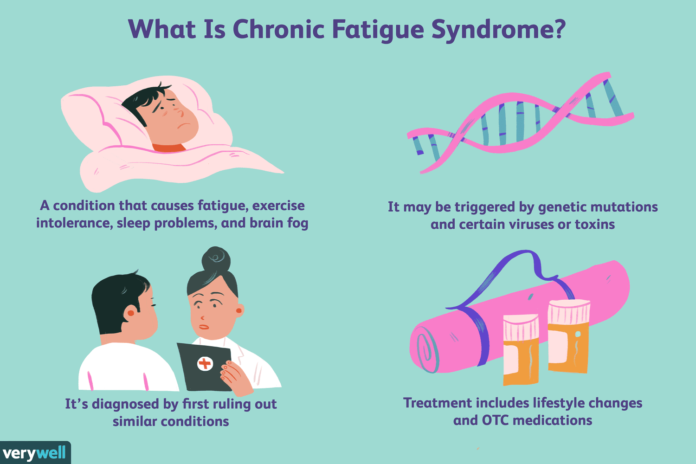
Syndrome of Chronic Fatigue
What is the syndrome of chronic fatigue?
Chronic fatigue syndrome, or CFS, is not the typical ups and downs of daily living. A strong and obvious exhaustion that often comes on quickly and either never stops or comes and goes is the early indicator of this sickness. Bed rest does not help it, and physical or mental activity may make it worse. Most of the time, people with CFS operate at a significantly reduced level of activity compared to their pre-illness capabilities. Women are diagnosed with CFS two to four times more frequently than men, presumably as a result of biological, psychological, and social factors.
Which indications and symptoms correspond to Chronic Fatigue Syndrome?
Two requirements must be met by the patient in order for CFS to be diagnosed. Clinical diagnostics must rule out other recognized medical diseases and indicate that the severe chronic fatigue persisted for at least six months. Significant impairment in short-term memory or concentration; sore throat; tender lymph nodes; muscle pain; multi-joint pain without swelling or redness; headaches of a new kind, pattern, or intensity; unrefreshing sleep; and post-exertional malaise lasting longer than 24 hours are additional requirements. The symptoms could not have preceded the exhaustion and had to have continued or returned for at least six months.
What leads to the syndrome of chronic fatigue?
Even after a thorough investigation, the cause(s) of CFS are still unknown. It is possible that CFS is a disease endpoint that arises from a variety of triggering factors. Viral infections or other brief traumatic events, stress, and toxins are a few of the causes that have been linked to the development of CFS.
Exist any risk factors?
According to research, women are more likely than males to experience CFS, and those in their 40s and 50s are the age group most afflicted.
Exists a therapy program?
For yet, there is no treatment for CFS. The goal of this disorder’s therapy is to reduce symptoms. Because too much stress can exacerbate the symptoms of CFS, it’s critical to maintain excellent health by eating a balanced diet, getting enough sleep, exercising frequently without becoming more fatigued, and taking it slow. Creating a regimen with a doctor in order to maximize benefits will also help you feel less frustrated with your sickness.
Acupuncture, aquatic therapy, chiropractic care, cranial-sacral therapy, light exercise, massage, self-hypnosis, tai chi, stretching, yoga, and therapeutic touch are examples of non-pharmacological therapies. Some psychotherapies, like cognitive behavioral therapy, have also demonstrated potential in helping patients cope and reducing some of the discomfort related to CFS.
Many drugs are available in pharmacological therapy to treat particular ailments. It’s crucial to start with modest dosages and increase them gradually as needed.
Joining a local CFS support group is one way for those with CFS to meet others who share their illness, which may also be therapeutic for some patients. Not everyone should attend support groups; in fact, they could make them feel more stressed than before.
The prognosis: what is it?
The disorder’s clinical course varies greatly throughout CFS patients. Even the notion of what constitutes recovery is up for controversy, as is the true percentage of patients who make a full recovery. While some people make enough progress to be able to return to work and other activities, they nevertheless occasionally or otherwise have CFS symptoms. Over time, some people fully recover, while others get worse and worse. The course of CFS is cyclical, with intervals of illness and periods of relative well-being.