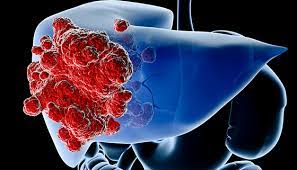
Cancer that starts in the cells of your liver is known as liver cancer. Located in the top right section of your abdomen, beneath your diaphragm and above your stomach, lies your liver, an organ the size of a football.
The liver can develop into several forms of cancer. Hepatocellular carcinoma is the most prevalent kind of liver cancer, and it starts in the primary hepatocyte form of liver cell. Hepatoblastoma and intrahepatic cholangiocarcinoma are two less prevalent forms of liver cancer.
Compared to cancer that starts in the liver cells, cancer that spreads to the liver occurs more frequently. Metastatic cancer, as opposed to liver cancer, is the term for cancer that starts in another part of the body, such as the colon, lung, or breast, and then spreads to the liver. This kind of cancer is called after the organ in which it first appeared; for example, cancer that starts in the colon and travels to the liver is called metastatic colon cancer.
Symptoms
In the early stages of primary liver cancer, the majority of people don’t exhibit any symptoms or indicators. When symptoms do materialise, they could include the following:
- losing weight naturally
- diminished appetite
- upper abdomen discomfort
- vomiting and queasiness
- overall weakness and exhaustion
- abdominal edoema
- jaundice is the yellow staining of the whites of your eyes and skin.
- chalky white stools
Causes
It happens when liver cells develop changes (mutations) in their DNA. A cell’s DNA is the material that provides instructions for every chemical process in your body. DNA mutations cause changes in these instructions. One result is that cells may begin to grow out of control and eventually form a tumor — a mass of cancerous cells.
Sometimes the cause of liver cancer is known, such as with chronic hepatitis infections. But sometimes liver cancer happens in people with no underlying diseases and it’s not clear what causes it.
Prevention
Lower your chance of developing cirrhosis
Liver cancer risk is increased by cirrhosis, which causes scarring of the liver. You can lower the chance of developing cirrhosis if you:
- If you use alcohol at all, do it in moderation. If you decide to consume alcohol, keep your intake to a minimum. This translates to women having no more than one drink each day. This translates to guys having no more than two drinks each day.
- Sustain an appropriate weight. If you are currently at a healthy weight, make an effort to stay there by eating well and doing exercise most days of the week. Lower your daily calorie intake and up your workout regimen if you need to shed some weight.
Obtain a hepatitis B vaccine.
Getting vaccinated against hepatitis B can lower your risk of contracting the disease. Nearly everyone can receive the vaccination, including young children, elderly people, and people with weakened immune systems.
Prevent hepatitis C by taking precautions.
Hepatitis C has no known vaccination, but you can lower your chance of contracting the illness.
Any sexual partner’s health status should be known. Until you are positive that your partner is free of HBV, HCV, or any other sexually transmitted virus, never have unprotected intercourse. Use a condom each and every time you engage in sexual activity with someone you don’t know well.
Avoid using intravenous (IV) medications, but if you must, make sure the needle is clean. Ease your risk of HCV by abstaining from drug injection. If that’s not an option for you, however, make sure that any needle you use is sterile and dispose of it properly. An infection with hepatitis C is frequently caused by tainted medication accessories. Use the needle-exchange services in your area, and think about getting drug treatment.
When getting a tattoo or getting pierced, look for clean, safe shops. Unsterilized needles have the potential to transmit the hepatitis C virus. Examine local stores for piercings and tattoos and inquire with staff about their safety procedures before having one. You can tell if a store isn’t the proper place for you if the staff doesn’t want to talk to you or doesn’t think your queries are important.
Seek medical attention if you have hepatitis B or C.
Both hepatitis B and hepatitis C illnesses have treatments available. Treatment can lower the risk of liver cancer, according to research.
Consult your doctor about screening for liver cancer.
It is not usually advised to screen for liver cancer in the general population as there is no evidence that doing so lowers the chance of dying from the disease. Individuals who have any of the following conditions that raise their risk of liver cancer should think about getting screened:
- Hepatitis B virus
- Hepatitis C virus
- Hepatic cirrhosis
Examine the benefits and drawbacks of screening with your physician. Based on your risk, you can determine together if screening is appropriate for you. Every six months, a blood test and an abdominal ultrasound examination are usually part of the screening process.