Acid reflux from the stomach constantly running back into the oesophagus, the tube that connects your mouth and stomach, is known as gastroesophageal reflux disease (GERD). The lining of your oesophagus may become irritated by this backwash, or acid reflux.
Periodically, a lot of people experience acid reflux. GERD can develop, though, if acid reflux occurs frequently over an extended period of time.
With medication and lifestyle modifications, the majority of people are able to control their GERD discomfort. Even though it’s rare, some people may require surgery to relieve their symptoms.
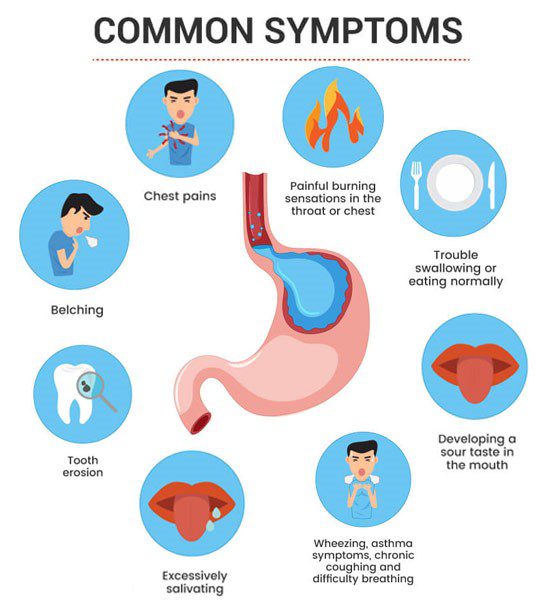
Symptoms of Gastroesophageal Reflux Disease (GERD)
Typical GERD symptoms and indicators include:
- heartburn is a burning feeling in your chest that usually occurs after eating and may be worse at night or when you’re lying down.
- regurgitating food or sour liquids, or backwashing
- chest or upper abdomen pain
- difficulty swallowing, or dysphagia
- feeling like there’s a lump in your throat
In addition to these symptoms, acid reflux during the night may also cause:
- A persistent cough
- Vocal cord inflammation (laryngitis)
- Asthma that is new or getting worse
Causes of Gastroesophageal Reflux Disease (GERD)
Frequent stomach acid reflux or reflux of nonacidic content is the cause of GERD.
The lower esophageal sphincter, a circular band of muscle that surrounds the bottom of your oesophagus, relaxes during swallowing to let food and liquids pass into your stomach. The sphincter then shuts once more.
Stomach acid can return to your oesophagus if the sphincter weakens or fails to relax as it should. The lining of your oesophagus becomes irritated by this continuous backwash of acid, frequently leading to inflammation.
Complications
Chronic esophageal inflammation over time can lead to:
Tissue inflammation in the oesophagus (esophagitis). Acid from the stomach can damage the tissue lining the oesophagus, leading to soreness, bleeding, and occasionally an ulcer. Swallowing can be painful and challenging if you have esophagitis.
The oesophagus becoming narrower (esophageal stricture). Scar tissue develops when stomach acid damages the lower oesophagus. The food pathway is narrowed by the scar tissue, which causes swallowing difficulties.
Barrett esophageal abnormalities caused by precancerous changes. Alterations in the tissue lining the lower oesophagus may result from acid damage. An increased risk of esophageal cancer is linked to these changes.
Treatment
It’s likely that your doctor will advise you to start with nonprescription medications and lifestyle modifications. Within a few weeks, if you still don’t feel better, your doctor may suggest further testing and prescription medication.
Over-the-counter drugs
Choices consist of:
Stomach acid-neutralizing antacids. Calcium carbonate-containing antacids, like Mylanta, Rolaids, and Tums, may offer immediate relief. However, an irritated oesophagus harmed by stomach acid cannot be healed by antacids alone. Certain antacid overuse can have negative side effects, like diarrhoea or occasionally kidney issues.
Drugs that lessen the production of acid. These drugs are referred to as histamine (H-2) blockers, and they include nizatidine (Axid AR), famotidine (Pepcid AC), and cimetidine (Tagamet HB). H-2 blockers don’t work as fast as antacids, but they last longer and can stop the stomach from producing acid for up to 12 hours. Prescriptions are available for stronger versions.
Drugs that treat the oesophagus and prevent the production of acid. These drugs, also referred to as proton pump inhibitors, are more potent acid blockers than H-2 blockers and give injured esophageal tissue more time to heal. Proton pump inhibitors available without a prescription include omeprazole (Prilosec OTC), lansoprazole (Prevacid 24 HR), and esomeprazole (Nexium 24 HR).
Prescription drugs
Treatments for GERD that come with a prescription include:
Proton pump inhibitors with prescription strength. These consist of pantoprazole (Protonix), rabeprazole (Aciphex), omeprazole (Prilosec), lansoprazole (Prevacid), and dexlansoprazole (Dexilant).
These drugs, while usually well tolerated, can occasionally result in low magnesium or vitamin B-12 levels, headaches, nausea, and diarrhoea.
H-2 blockers with prescription strength. These include nizatidine and famotidine at prescription strength. These drugs typically have mild, well-tolerated side effects.
Procedures such as surgery
Medication is typically effective in controlling GERD. However, if drugs are ineffective for you or you would prefer not to take medications over the long term, your doctor may advise:
Fundoplication. In order to tighten the muscle and stop reflux, the surgeon wraps the upper portion of your stomach around the lower esophageal sphincter. Laparoscopic surgery, which is minimally invasive, is typically used to perform fundoplications. Partial or complete wrapping of the upper portion of the stomach is possible (Nissen fundoplication). The Toupet fundoplication is the most frequently performed partial procedure. Your surgeon will advise you on the best type for you.
LINX apparatus. The esophageal-gastric junction is encircled by a ring of tiny magnetic beads. Although the magnetic attraction between the beads is weak enough to let food pass through, it is strong enough to keep the junction closed against acid reflux. A minimally invasive surgical procedure can be used to implant the LINX device. Magnetic resonance imaging and airport security are unaffected by the magnetic beads.
Transoral fundoplication without incision (TIF). Using polypropylene fasteners to partially wrap the lower oesophagus, this new procedure tightens the lower esophageal sphincter. TIF doesn’t require a surgical incision because it is done through the mouth with an endoscope. Its benefits include high tolerance and a short recovery period.
TIF by itself is not a viable option if you have a large hiatal hernia. On the other hand, TIF might be feasible in conjunction with laparoscopic hiatal hernia repair.
Your healthcare professional may recommend weight-loss surgery as a treatment option for GERD because obesity can be a risk factor for the condition. Find out if you qualify for this kind of surgery by speaking with your provider.