Psoriatic arthritis is a type of arthritis that some people with psoriasis (a skin condition characterised by red skin patches covered in silvery scales) experience. Before being diagnosed with psoriatic arthritis, the majority of people first develop psoriasis. However, for some, the joint issues start concurrently with or before the skin patches do.
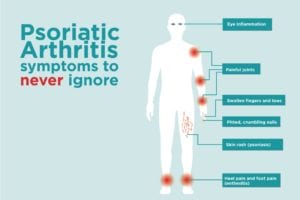
The primary indicators and symptoms of psoriatic arthritis are joint pain, stiffness, and swelling. They can range in severity from mild to severe and affect any part of the body, including your fingertips and spine. Periods of remission can alternate with flare-ups of the disease in both psoriasis and psoriatic arthritis.
It is not possible to treat psoriatic arthritis. The goals of treatment are to manage symptoms and avoid joint deterioration. Psoriatic arthritis can be very debilitating if left untreated.
Symptoms
Psoriasis and psoriatic arthritis are both long-term conditions that get worse with time. On the other hand, there may be times when your symptoms get better or disappear entirely.
One or both sides of your body’s joints may be impacted by psoriatic arthritis. Psoriatic arthritis symptoms and indicators are frequently confused with rheumatoid arthritis symptoms. Joints affected by these conditions experience pain, swelling, and warmth when touched.
But psoriatic arthritis also has a higher likelihood of causing:
Swollen toes and fingers. Your fingers and toes may swell painfully and sausage-like as a result of it.
Foot ache. Additionally, it can cause pain at the sites where ligaments and tendons attach to your bones. This is particularly common in plantar fasciitis and Achilles tendinitis, which affect the soles of your feet and the back of your heel, respectively.
Back pain in the lower back. As a consequence of psoriatic arthritis, some people get spondylitis. The primary symptoms of spondylitis are inflammation of the joints in your spine between the vertebrae and in your pelvis (sacroiliitis).
Nails shift. Little pits, crumbling, or separation from the nail beds are all possible with nails.
Inflammation of the eyes. Redness, pain, and blurred vision are some of the symptoms of uveitis. Untreated uveitis can result in blindness.
Causes
When your body’s immune system targets healthy cells and tissue, it can lead to arthritis. The immune response results in both an excess of skin cells and joint inflammation.
It appears likely that this immune system response is influenced by both environmental and genetic factors. A family history of psoriasis or psoriatic arthritis is common among those who suffer from psoriatic arthritis. Certain genetic markers that seem to be connected to psoriatic arthritis have been found by researchers.
In those with a genetic predisposition, it may be brought on by physical trauma or environmental factors, such as a bacterial or viral infection.
Treatment
There’s no treatment for it. In order to prevent joint pain and disability, treatment focuses on reducing inflammation in the affected joints as well as skin involvement. Prescription medications known as disease-modifying antirheumatic drugs (DMARDs) are among the most widely used forms of treatment.
The severity of your condition and the joints that are impacted will determine how you are treated. It may take trying a few different treatments before you find one that relieves your symptoms.
Drugs
Medications include:
- NSAIDs. For those with mild psoriatic arthritis, nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce inflammation and relieve pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) like naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, and other brands) are available over-the-counter. Prescriptions are available for stronger NSAIDs. Damage to the kidneys and liver, as well as heart issues, can be side effects.
- Traditional DMARDs, or disease-modifying antirheumatic medications.
These medications can prevent irreversible damage to joints and other tissues by delaying the course of psoriatic arthritis.
Trexall, Otrexup, and methotrexate are among the brand names for the disease-modifying antirheumatic drug (DMARD) that is most utilised. Leflunomide (Arava) and sulfasalazine (Azulfidine) are two more. Liver damage, suppression of the bone marrow, lung inflammation, and scarring (fibrosis) are possible side effects.
- Biological agents. This class of DMARD, also referred to as biologic response modifiers, targets various immune system pathways. Adalimumab (Humira), ixekizumab (Taltz), guselkumab (Tremfya), golimumab (Simponi), etanercept (Enbrel), infliximab (Remicade), ustekinumab (Stelara), secukinumab (Cosentyx), and abatacept (Orencia) are examples of biologic agents. These medications may make infections more likely.
- Focused on artificial DMARDs. In cases where biologic agents and conventional DMARDs have failed, tofacitinib (Xeljanz) may be used. Elevated tofacitinib dosages may raise the risk of lung blood clots, major cardiac events, and cancer.
- Modern oral drugs. The body’s enzyme that regulates the level of inflammation within cells is less active when taken as part of apremilast (Otezla). When treating mild to moderate psoriatic arthritis, apremilast is used for patients who cannot or should not take biologics or DMARDs. Headaches, nausea, and diarrhoea are possible side effects.
Treatments
Occupational and physical therapy may reduce pain and facilitate daily activities. Get recommendations from your physician. Additionally, massage therapy may provide relief.
Procedures such as surgery
- Injections of steroids. Inflammation in an afflicted joint can be decreased with injections.
- Surgery to replace a joint. It is possible to replace some severely damaged joints caused by psoriatic arthritis with metal and plastic artificial joints.