You may have an arrhythmia if your heart rhythm is abnormal or if the pace of your heartbeat is abnormal. Different types of arrhythmias have different names based on the location of the abnormality in the heart and its underlying cause. Your heart is pounding too quickly if you have tachycardia. When at rest, it can reach over 100 beats per minute.
Your upper heart chambers are where your rapid heartbeat starts when you have supraventricular tachycardia, or SVT. The heart’s electrical signals and circuitry malfunction is the root reason. It is difficult to pump enough blood to your body when your heart beats too quickly because it cannot fill with blood between beats.
Consider it this way: People won’t have enough time to enter the elevator before the doors close if they close too quickly. Similar to this, an excessively rapid heartbeat prevents the heart chambers from contracting before the blood has had a chance to fill them.
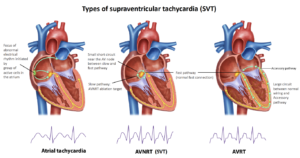
There are various varieties of supraventricular tachycardia, or SVT. They are as follows:
- Premature contractions of the atrium (PACs).
- PSVT stands for paroxysmal supraventricular tachycardia.
- Tachycardias caused by accessory pathways, such Wolff-Parkinson-White (WPW)
- syndrome.
- AVNRT stands for atrioventricular nodal re-entrant tachycardia.
- Tachycardia atrial.
- Fibrillation of the heart.
- Fluttering of the atrium.
Who is affected by supraventricular tachycardia (SVT)?
Supraventricular tachycardia, or SVT, can strike both adults and children. More women than males understand it. Some have a higher risk of developing this illness because they:
- Feel uneasy.
- Consume more alcohol than what your supplier has advised.
- Use tobacco goods or smoke.
- Consume more coffee or other caffeinated beverages than is advised.
Teenagers who engage in intense physical activity have the risk of experiencing short-term paroxysmal supraventricular tachycardia (PSVT). In young people and the elderly, AV (atrioventricular) nodal reentrant tachycardia) is prevalent. In children under the age of twelve, accessory pathway tachycardias, including WPW syndrome, are prevalent.
Premature atrial contractions (PACs) are more common in the elderly, agitated, and over-caffeinated populations. Atrial flutter is more common in older adults, diabetics, and people with lung diseases. Caffeine, alcohol, heart illness, and lung disease increase the risk of atrial tachycardia. Atrial fibrillation is also more common in those with heart and lung conditions.
How frequent is supraventricular tachycardia, or SVT?
2.25 persons out of every 1,000 had SVT (supraventricular tachycardia).
Signs and Origins
Why does supraventricular tachycardia, or SVT, occur?
SVT is caused by an issue with the electrical signals or circuitry of your heart, though some individuals may not be aware of the exact reason of their symptoms. Some people’s SVT is clearly initiated by a “trigger,” such as stress or physical activity. The following are some things that can cause symptoms:
- Heartbeats in excess.
- Tension.
- Coffee.
- Booze.
- Smoke from cigarettes.
- SVT can also occur in pregnant women and those with thyroid, lung, or heart conditions.
What signs of supraventricular tachycardia, or SVT, are present?
Even though you may not be experiencing any symptoms, a rapid heartbeat of greater than 100 beats per minute during rest is a common symptom for many people. This may continue for a few seconds or for several hours. Additional signs and symptoms could be:
- Experiencing ache in the chest.
- I’m worn out.
- Enduring a rapid pulse.
- I’m dizzy.
- Perspiration.
- I’m experiencing vertigo.
- Fading away.
- Experiencing palpitations, or chest flutters.
- Breathing heavily.
- Individuals experiencing a severe case may pass out or experience cardiac arrest.
Diagnoses and Examinations
How is supraventricular tachycardia, or SVT, identified?
It’s likely that your doctor will do an electrocardiogram (ECG, often known as an EKG). Your doctor can ask you to wear a heart monitor, which captures the electrical activity in your heart, if they need to examine your heart for a longer period of time.