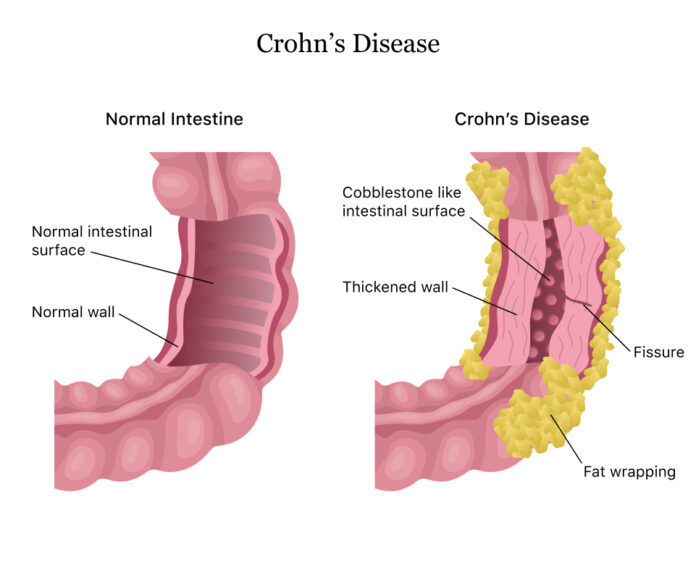
One kind of inflammatory bowel disease (IBD) is Crohn’s disease. It results in inflammation (swelling of the digestive tract tissues), which can cause severe diarrhoea, exhaustion, weight loss, and malnourishment in addition to abdominal pain.
Crohn’s disease-related inflammation typically affects the small intestine but can affect other parts of the digestive tract in different individuals. It is common for this inflammation to extend into the bowel’s deeper layers.
In addition to being crippling and painful, Crohn’s disease can occasionally result in potentially fatal complications.
Although Crohn’s disease has no known cure, treatments can significantly lessen its symptoms, even induce a long-term remission, and help the inflammation heal. Many people with Crohn’s disease are able to lead normal lives after receiving treatment.
Symptoms
Any area of your small or large intestine may be affected by Crohn’s disease. It could be in one continuous piece or divided into several segments. In certain individuals, the illness solely affects the colon, which is a section of the large intestine.
Crohn’s disease can cause mild to severe signs and symptoms. Though they often appear gradually, they can occasionally appear suddenly and without warning. Additionally, there can be times when you exhibit no symptoms at all (remission).
Symptoms that usually appear when the illness is active include:
- The diarrhoea
- High temperature
- Weary
- Cramping and pain in the abdomen
- Your stool contains blood
- Oral sores
- Decreased hunger and loss of weight
- Anus pain or discharge around the anus as a result of inflammation from a fistula, a tunnel that enters the skin
Additional indications and symptoms
Severe Crohn’s disease patients may also have symptoms that are not limited to the gastrointestinal tract, such as:
- inflammation of the eyes, joints, and skin
- inflammation of the bile ducts or liver
- kidney stones
- low iron levels (anaemia)
- delayed sexual development or growth in children
Causes
We still don’t know the precise cause of Crohn’s disease. Although stress and food were once thought to be contributing factors, medical professionals now understand that these things only worsen Crohn’s disease. Its development most likely stems from a number of factors.
Immune system. There’s a chance that a virus or bacteria could cause Crohn’s disease, but researchers haven’t found one yet. An atypical immune response leads your immune system to attack the cells in your digestive tract as well as the invasive microorganism or environmental trigger.
Genetics. Genes may contribute to an individual’s increased risk of developing Crohn’s disease, as the condition is more prevalent in those who have family members who have it. Nonetheless, the majority of Crohn’s disease sufferers do not have a family history of the condition.
Treatment
Crohn’s disease does not currently have a cure, nor is there a single effective treatment. Reducing inflammation is one of the main objectives of medical treatment, as it causes your symptoms and signs. Reducing complications has the additional objective of improving the long-term prognosis. In the best circumstances, this could result in a long-term remission in addition to symptom relief.
Anti-inflammatory medications
When treating inflammatory bowel disease, anti-inflammatory medications are frequently used initially. Among them are:
Steroids. While corticosteroids, like budesonide (Entocort EC) and prednisone, can help lower inflammation in the body, not everyone with Crohn’s disease responds well to them.
Corticosteroids can be used to induce remission and improve symptoms for a brief period of time (3 to 4 months). Moreover, corticosteroids can be taken in conjunction with immune system suppressors to enhance the effects of other drugs. After that, they gradually taper off.
5-aminosalicylates orally. In general, these medications don’t help people with Crohn’s disease. These include mesalamine (Delzicol, Pentasa, etc.) and sulfasalazine (Azulfidine), which contains sulfa. Although oral 5-aminosalicylates were once extensively used, they are now generally regarded as having very little benefit.
Suppressors of the immune system
These medications also lessen inflammation, but they do so by attacking your immune system, which is the source of the inflammatory chemicals. Some people respond better to a combination of these medications than to each one taken alone.
Suppressors of the immune system include:
Mercaptopurine (Purinethol, Purixan) and azathioprine (Azasan, Imuran). When treating inflammatory bowel disease, these are the immunosuppressants that are most frequently used. If you take them, you must closely monitor your progress with your physician and undergo routine blood work to check for adverse effects, such as decreased immune response and hepatic inflammation. They might also make you feel queasy or throw up.
Antibiotics
In patients with Crohn’s disease, antibiotics can sometimes cure fistulas and abscesses and lessen their drainage. Additionally, some scientists believe that antibiotics aid in the reduction of pathogenic bacteria that might be responsible for intestinal inflammation. Metronidazole (Flagyl) and ciprofloxacin (Cipro) are two commonly prescribed antibiotics.
Diet therapy
If you have Crohn’s disease, your doctor might suggest parenteral nutrition—nutrients injected into a vein—or an exclusive diet administered orally or through a feeding tube. This can help you eat better overall and give your intestines a break. In the short term, bowel rest may help to reduce inflammation.
Your physician may prescribe immune system suppressors along with nutrition therapy for a brief period of time. When other medications are unable to control symptoms, people are often put on enteral or parenteral nutrition to help them get healthier before surgery.
If you have a narrowed bowel (stricture), your doctor might also suggest a low-residue or low-fiber diet to lower your risk of intestinal blockage. The goal of a low residue diet is to minimise the quantity and size of your faeces.
Operation
Your doctor might suggest surgery if medication therapy, dietary and lifestyle modifications, or other treatments are ineffective in relieving your symptoms. Almost 50% of people with Crohn’s disease will need surgery at least once. Nevertheless, Crohn’s disease cannot be cured by surgery.
Your digestive tract’s damaged sections are removed during surgery, and the healthy sections are reconnected. Draining abscesses and sealing fistulas can both be done surgically.
Surgery for Crohn’s disease typically has short-term benefits. The illness frequently returns, usually in the vicinity of the repaired tissue. To reduce the chance of a recurrence, the best course of action is to take medication after surgery.