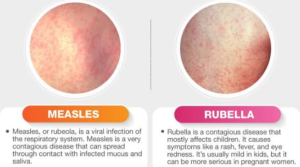
What is Rubella?
The viral infection rubella causes a rash or skin eruption. When an infant or toddler contracts the illness, the rash and other symptoms are typically fairly mildly shown. However, children who acquire the disease from their mother while she is expecting can experience severe birth abnormalities in addition to other negative effects. Women who are pregnant and have been exposed to rubella should get help right once.
-
Rubella is caused by a virus known as a rubivirus.
-
It can be passed from a pregnant woman to her unborn child or through contact with the secretions of another sick individual . Children can contract rubella through direct contact with nasal and oral secretions.
-
By receiving the appropriate rubella vaccination, rubella can be avoided.
Signs & Causes
What causes rubella?
Rubella is caused by a virus known as a rubivirus. It can be passed from a pregnant woman to her unborn child or by the secretions of another infected individual. In the late winter and early spring, it is most common. Rubella is preventable through immunization with the rubella vaccine, which is one of the recommended immunizations that your child should take during annual checkups.
Are there any severe repercussions?
When an infant or toddler contracts the illness, the rash and other symptoms are typically fairly moderate. However, children who acquire the disease from their mother while she is expecting can experience severe birth abnormalities in addition to other negative effects. It’s especially risky for pregnant women to come into contact with someone who has rubella because it can lead to miscarriage.
WARNING: Pregnant women who have been exposed to rubella should seek medical assistance immediately.
There are no long-term effects of the disease itself. Preventing an infectious child from infecting a pregnant lady is the main worry.
What are the symptoms of rubella?
It may take 14 to 21 days for a kid to develop symptoms of rubella after coming into contact with the disease, but it is vital to remember that a child is most contagious when the rash is erupting. However, the youngster may be contagious beginning 7 days before the rash appears and continuing for 7 to 14 days after the rash appears. Your child could be contagious before you realize he or she has the sickness.
Each child will have distinct symptoms, however the following are the most prevalent indicators of childhood rubella:
-
A period of being unwell, accompanied by diarrhea and a low-grade temperature. This could last from one to five days.
-
The rash then develops as a pink rash with patches of tiny, elevated lesions.
- A rash that
starts on the face and moves down the body, down the arms, and down the legs.
-
The rash on the face normally improves as the rash extends to the arms and legs.
-
The rash normally disappears between the third and fifth day.
-
Lymph nodes in the neck may also swell.
-
Older children and teenagers may experience joint pain and inflammation.
Congenital rubella, which occurs at birth because the child caught it from his mother while in gestation, can also cause the following complications:
-
Cataracts in the eyes
-
heart problems
-
mental retardation
-
retardation growth
-
enlarged liver and spleen
-
skin lesions
-
bleeding problems
Prevention of rubella
“We are seeing these new “pockets” or clusters of decreased vaccination, which are fueling outbreaks,” says Ronald Samuels, MD, MPH. “Measles is extremely contagious; it only needs a few cases to spread like wildfire.”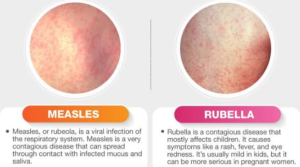
Since the rubella vaccination was developed, the disease’s occurrence has dropped by more than 99 percent. Nowadays, adults without vaccinations account for the majority of cases.
The MMR vaccine, which also contains the measles, mumps, and rubella vaccines, is typically administered together. It is usually administered when your child is 12 to 15 months old, and then again when he or she is 4 to 6 years old. If your child has not received the second dose by the age of 6, he or she should do so by the age of 11 or 12. Girls should also have their rubella vaccinations prior to becoming pregnant.
“When people opt out [of the vaccine], they substantially raise the chance that measles will be transmitted around the community, not only to their child, but to children who can’t be vaccinated, or to the small number of children for whom the vaccine just doesn’t work,” states Ronald Samuels, MD, MPH. The youngest children under 1 who have not yet had standard vaccinations are the ones who are most at danger.
“Parents worry about their children with good reason. If you’re not concerned about your child, you’re not being a decent parent. “However, people underestimate the disease’s dangers,” says Ronald Samuels, MD, MPH. “They say it’s 10 days of fever; well, it’s 10 days of fever unless your child dies.” What would you do if I told you that your child has a one in 1,000 chance of dying? You’re betting not that the condition is minor, but that your child will not acquire it. The danger increases significantly if parents choose not to vaccinate their children against the disease.
Added measures to stop the spread of rubella include:
-
Seven days after the rash appears, kids shouldn’t go to school.
-
Rubella is considered contagious for the first year of life in newborns.
-
Verify that all of your child’s contacts have had the appropriate vaccinations.
Diagnosis & Treatments
How is rubella diagnosed?
Rubella is often diagnosed through a medical history and physical examination of your child. Because each rubella lesion is distinct, your child’s doctor can usually make a diagnosis based on a basic physical examination. Your child’s doctor may also order blood or urine tests to confirm the diagnosis.
Because rubella is a viral infection, there is no cure. The goal of treatment is to either prevent the disease from occurring in the first place or to reduce the severity of the symptoms.
Treatment may include:
-
increased fluid intake.
-
rest.
-
isolation to prevent spread of the virus.