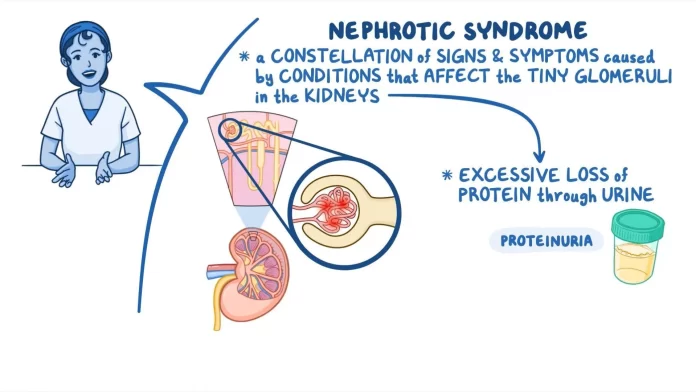
Nephritic syndrome is a kidney condition involving inflammation of the glomeruli, which are the tiny blood vessels in the kidneys responsible for filtering waste and excess fluids. When these glomeruli become inflamed, kidney function is impaired, leading to various symptoms.
Symptoms of Nephritic Syndrome:
- Hematuria: Blood in the urine, often visible as cola-colored or dark urine.
- Proteinuria: Mild to moderate levels of protein in the urine.
- Hypertension: High blood pressure due to fluid retention.
- Edema: Swelling in the face, particularly around the eyes, as well as in the feet and ankles.
- Oliguria: Reduced urine output.
- Azotemia: Accumulation of nitrogenous wastes (such as urea) in the blood.
- Flank pain: Some individuals experience discomfort or pain in the lower back or side.
Causes of Nephritic Syndrome:
It is usually secondary to other diseases or conditions, and its causes are often immune-related or infectious:
- Post-Streptococcal Glomerulonephritis: Often occurs after a throat or skin infection caused by Streptococcus bacteria.
- Lupus Nephritis: Associated with systemic lupus erythematosus (SLE), an autoimmune disorder.
- IgA Nephropathy (Berger’s Disease): Involves the buildup of immunoglobulin A (IgA) in the kidneys.
- Goodpasture Syndrome: An autoimmune condition where antibodies attack the kidneys and lungs.
- Vasculitis: Inflammation of blood vessels, affecting kidney function (e.g., ANCA-associated vasculitis).
- Membranoproliferative Glomerulonephritis (MPGN): A type of kidney inflammation that can lead to nephritic syndrome.
- Infectious Diseases: Certain viral or bacterial infections may trigger nephritic syndrome.
- Alport Syndrome: A genetic disorder affecting the kidneys, ears, and eyes.
Treatment of Nephritic Syndrome:
The treatment depends on the underlying cause but may include:
- Control of Blood Pressure: Using antihypertensive medications, especially ACE inhibitors or ARBs (angiotensin receptor blockers).
- Diuretics: To reduce fluid buildup and manage edema.
- Corticosteroids: To reduce inflammation in cases of autoimmune causes.
- Immunosuppressive Therapy: Drugs like cyclophosphamide or rituximab may be used in cases of severe autoimmune-related nephritic syndrome.
- Antibiotics: If the condition is related to a bacterial infection, antibiotics may be prescribed.
- Dialysis: In cases of acute kidney failure, dialysis may be necessary to remove waste products and excess fluids.
- Plasmapheresis: Used in conditions like Goodpasture syndrome, where antibodies need to be removed from the blood.
Prevention of Nephritic Syndrome:
While it may not always be possible to prevent nephritic syndrome, especially if it arises from genetic or autoimmune conditions, certain preventive measures can help reduce the risk:
- Treat Infections Promptly: Proper treatment of streptococcal infections can help prevent post-streptococcal glomerulonephritis.
- Manage Autoimmune Diseases: Keeping autoimmune conditions like lupus under control can lower the risk of nephritic syndrome.
- Avoid Risky Medications and Toxins: Certain drugs or toxic substances can damage the kidneys.
- Control High Blood Pressure and Diabetes: These conditions can worsen kidney function and should be well-managed to reduce kidney damage.
- Healthy Lifestyle: Regular exercise, a balanced diet, and avoiding excessive salt intake can help maintain kidney health.
Prognosis:
The prognosis for nephritic syndrome varies depending on the cause and how early it is diagnosed and treated. In some cases, the inflammation resolves with proper treatment, while in others, it may lead to chronic kidney disease or kidney failure.