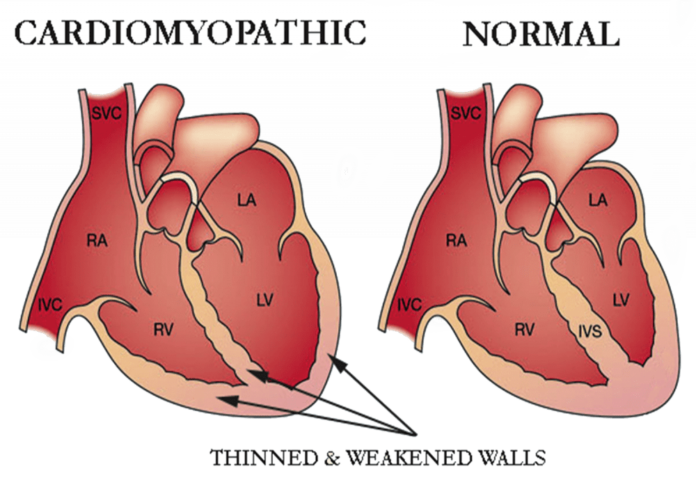
Cardiomyopathy refers to diseases of the heart muscle that can lead to a decrease in the heart’s ability to pump blood effectively. This can result in heart failure and other serious complications. There are several types of cardiomyopathy, each with different causes and treatment approaches.
Symptoms
Symptoms of cardiomyopathy can vary depending on the type and severity of the condition but commonly include:
- Shortness of breath: Especially with physical activity or when lying flat.
- Fatigue: Feeling unusually tired or weak.
- Swelling: In the legs, ankles, or abdomen.
- Palpitations: Irregular or rapid heartbeats.
- Chest pain: Though less common, some may experience discomfort or pain.
- Dizziness or fainting: Particularly if there are issues with heart rhythm or severe heart failure.
Causes
The causes of cardiomyopathy can be broadly categorized into primary (genetic or idiopathic) and secondary (resulting from another condition):
- Primary Cardiomyopathies:
- Genetic: Many forms are inherited, such as hypertrophic cardiomyopathy (HCM) or dilated cardiomyopathy (DCM).
- Idiopathic: Sometimes, no specific cause can be identified.
- Secondary Cardiomyopathies:
- Ischemic Cardiomyopathy: Resulting from coronary artery disease or a history of heart attacks.
- Hypertensive Cardiomyopathy: Caused by high blood pressure.
- Infectious: Viral infections can lead to myocarditis, which can evolve into cardiomyopathy.
- Toxic: Exposure to certain toxins or drugs, such as excessive alcohol or chemotherapy agents.
- Metabolic: Conditions like diabetes or thyroid disorders can impact heart muscle function.
- Pregnancy: Peripartum cardiomyopathy occurs during the last month of pregnancy or up to five months postpartum.
Treatment
Treatment for cardiomyopathy aims to manage symptoms, prevent complications, and improve the quality of life. The approach may include:
- Medications:
- ACE inhibitors or ARBs: To reduce blood pressure and heart strain.
- Beta-blockers: To manage heart rate and reduce the workload on the heart.
- Diuretics: To reduce fluid buildup and alleviate swelling.
- Antiarrhythmics: For managing irregular heartbeats.
- Anticoagulants: To prevent blood clots, particularly if there’s a risk of stroke.
- Lifestyle Changes:
- Dietary modifications: Reducing salt and alcohol intake.
- Exercise: As advised by a healthcare provider.
- Weight management: To alleviate additional stress on the heart.
- Medical Procedures:
- Implantable Cardioverter Defibrillator (ICD): For preventing sudden cardiac death.
- Pacemaker: To help regulate heart rhythms.
- Cardiac Resynchronization Therapy (CRT): For improving heart function in specific cases.
- Ventricular Assist Devices (VADs): To support heart function in advanced cases.
- Heart Transplant: In severe cases where other treatments are ineffective.
Prevention
While not all cases of cardiomyopathy are preventable, certain measures can help reduce the risk:
- Manage chronic conditions: Control high blood pressure, diabetes, and other underlying health issues.
- Avoid alcohol and drugs: Limit or avoid substances that can harm the heart muscle.
- Healthy lifestyle: Follow a balanced diet, exercise regularly, and maintain a healthy weight.
- Regular check-ups: For those with a family history or genetic predisposition, routine monitoring can help catch issues early.
If you suspect you have symptoms of cardiomyopathy or have a family history of the condition, it’s important to consult with a h