Chronic Obstructive Pulmonary Disease (COPD)
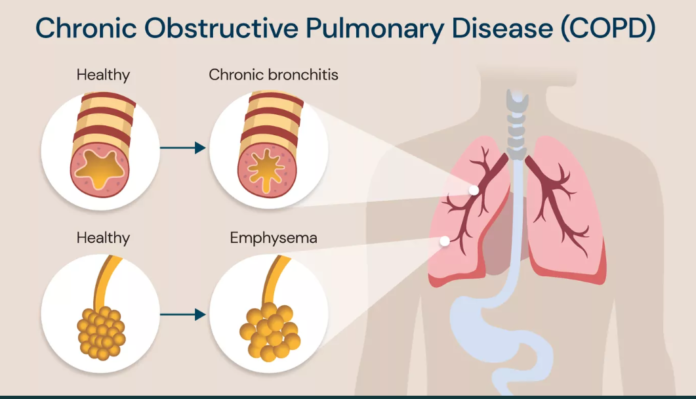
Chronic Obstructive Pulmonary Disease (COPD) is a progressive and debilitating respiratory condition characterized by persistent airflow limitation that is not fully reversible. It encompasses two main conditions: chronic bronchitis and emphysema, each contributing to the overall disease burden. COPD is a major global health problem, leading to significant morbidity, mortality, and healthcare costs. Understanding its pathophysiology, risk factors, symptoms, diagnosis, treatment, and management is crucial for improving patient outcomes and quality of life.
Pathophysiology
COPD is primarily caused by long-term exposure to harmful particles or gases, with cigarette smoking being the most common culprit. This exposure leads to chronic inflammation of the airways and lung tissues. In chronic bronchitis, the inflammation and subsequent mucus hypersecretion cause a persistent cough and expectoration of mucus. Emphysema involves the destruction of the alveoli, the tiny air sacs in the lungs, leading to decreased surface area for gas exchange.
The pathological changes in COPD include:
- Airway Inflammation: Chronic inflammation leads to thickening of the airway walls and increased mucus production, which narrows the airways and impairs airflow.
- Airway Remodeling: Structural changes in the airway, such as fibrosis and smooth muscle hypertrophy, contribute to persistent airflow limitation.
- Destruction of Alveoli: Emphysema results in the destruction of alveolar walls, causing loss of lung elasticity and impaired gas exchange.
These changes culminate in airflow obstruction, reduced oxygenation of blood, and difficulty in breathing, which are hallmark symptoms of COPD.
Risk Factors
The primary risk factor for COPD is smoking, which is responsible for the majority of COPD cases. Other risk factors include:
- Environmental Pollutants: Exposure to air pollution, occupational dusts, and fumes can contribute to the development of COPD.
- Genetic Factors: Alpha-1 antitrypsin deficiency is a rare genetic disorder that can lead to early onset emphysema.
- Age: COPD typically develops after many years of exposure to risk factors and is more common in older adults.
- Gender: Historically more common in men, the prevalence of COPD among women has increased due to rising smoking rates among women.
Symptoms
COPD symptoms often develop gradually and can be mistaken for other conditions. Common symptoms include:
- Chronic Cough: A persistent cough that lasts for three months or more.
- Sputum Production: Production of mucus, which may be thick and colored.
- Dyspnea: Shortness of breath, especially during physical activity or exertion.
- Wheezing: A high-pitched whistling sound when breathing, particularly during expiration.
- Fatigue: Feeling unusually tired or fatigued due to the increased effort of breathing.
As the disease progresses, symptoms can worsen, leading to frequent exacerbations and a significant impact on the patient’s daily activities and overall quality of life.
Diagnosis
Diagnosing COPD involves a combination of clinical evaluation, imaging, and pulmonary function tests:
- Medical History and Physical Examination: A detailed history of symptoms, smoking history, and exposure to risk factors is crucial. Physical examination may reveal wheezing, prolonged expiration, and decreased breath sounds.
- Spirometry: The most definitive test for diagnosing COPD, spirometry measures the volume and flow of air during inhalation and exhalation. The hallmark of COPD on spirometry is a reduced FEV1/FVC ratio (Forced Expiratory Volume in 1 second/Forced Vital Capacity).
- Imaging: Chest X-rays or computed tomography (CT) scans can help assess the extent of lung damage, identify other conditions, and differentiate between COPD and other respiratory diseases.
- Arterial Blood Gas Analysis: This test measures the levels of oxygen and carbon dioxide in the blood and helps assess the severity of the disease.
Treatment and Management
While there is no cure for COPD, management strategies focus on alleviating symptoms, improving quality of life, and slowing disease progression. Key components of COPD management include:
- Smoking Cessation: The most effective intervention for slowing the progression of COPD is quitting smoking. Nicotine replacement therapies, medications, and counseling can support smoking cessation efforts.
- Pharmacotherapy: Medications used in COPD include:
- Bronchodilators: These medications help relax and open the airways. They are categorized into short-acting (e.g., albuterol) and long-acting (e.g., salmeterol, tiotropium) types.
- Inhaled Corticosteroids: These reduce inflammation in the airways and are often used in combination with long-acting bronchodilators (e.g., fluticasone).
- Combination Inhalers: Some inhalers combine both bronchodilators and corticosteroids for more effective symptom control.
- Oxygen Therapy: For patients with severe COPD and low blood oxygen levels, supplemental oxygen can help improve oxygenation and reduce symptoms.
- Pulmonary Rehabilitation: A comprehensive program that includes exercise training, education, and support to help patients improve their physical endurance, manage symptoms, and enhance their quality of life.
- Vaccinations: Annual influenza vaccinations and pneumococcal vaccines are recommended to reduce the risk of respiratory infections and exacerbations.
- Surgical Interventions: In severe cases, surgical options such as lung volume reduction surgery or lung transplantation may be considered for patients who do not respond to other treatments.
Lifestyle Modifications
In addition to medical treatments, lifestyle changes play a crucial role in managing COPD:
- Physical Activity: Regular exercise can improve respiratory function and overall fitness. Tailored exercise programs can help patients maintain physical activity levels despite their limitations.
- Healthy Diet: A balanced diet can help maintain optimal body weight and support overall health. Malnutrition or obesity can negatively affect COPD management.
- Avoiding Respiratory Irritants: Patients should minimize exposure to pollutants, allergens, and other respiratory irritants to prevent exacerbations.
Prognosis and Outlook
COPD is a progressive disease with no cure, but with appropriate management, patients can lead active and fulfilling lives. The progression of COPD varies among individuals, and treatment aims to slow the progression, manage symptoms, and improve quality of life. Early diagnosis and intervention are crucial for better outcomes.
In conclusion, Chronic Obstructive Pulmonary Disease is a significant health challenge that requires a multifaceted approach to manage effectively. Understanding the disease’s pathophysiology, recognizing risk factors, and implementing comprehensive treatment and lifestyle strategies can help mitigate its impact and improve the lives of those affected. Ongoing research and advancements in medical care continue to offer hope for better management and potential future breakthroughs in the fight against COPD.