A brain-connected pacemaker presents hope for the treatment of depression. A novel brain pacemaker is opening the door to treating depression, which is a significant advancement in the field of mental health.
Deep Brain Stimulation, or DBS, has become a ray of hope for those suffering from severe depression that does not respond to conventional treatments. Emily Hollenbeck is one of them; she suffered from a crippling depression that was unabated by conventional therapies.
Her experience with DBS is representative of a larger story that offers hope to millions of others going through comparable difficulties.
HOW IS THE BRAIN PACEMAKER OPERATIONALLY?
The effectiveness of DBS, a treatment approved for diseases including epilepsy and Parkinson’s disease, is currently being investigated in the treatment of depression. By implanting electrodes in the brain, the procedure delivers precise electrical impulses that work similarly to a pacemaker but specifically for the brain.
Despite earlier failures in extensive investigations, this novel strategy has attracted interest because of its encouraging outcomes in more recent experiments.
Hollenbeck’s Mount Sinai West procedure experience highlights the therapy’s transforming power. She struggled with depression from childhood, which was made worse by her parents’ suicides, and when traditional therapies failed to provide long-lasting relief, she found herself in a difficult situation.
She was among the few hundred people treated for depression using DBS, having made the decision to have the procedure motivated by her desperate search for a way out.
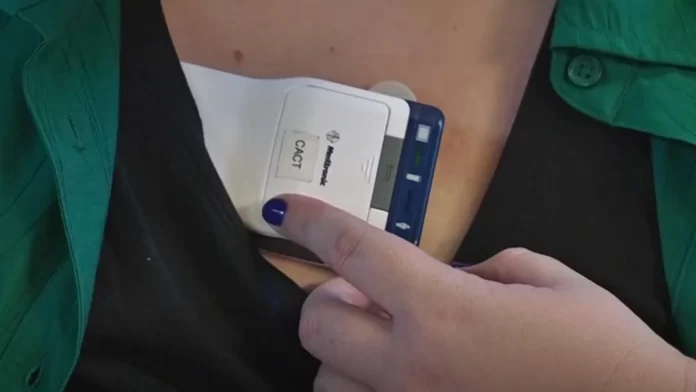
Thin metal electrodes were inserted during surgery into a particular part of the brain that controls emotional behavior. These electrodes are attached to an electrical stimulation control device that is implanted beneath the skin in the chest.
In order to restore normal neural activity, DBS helps “unstick” the brain’s emotional circuitry, according to Dr. Brian Kopell, head of Mount Sinai’s Center for Neuromodulation.
THE MAJOR CHANGE
Hollenbeck felt the instant and significant effects. She claimed that her depression symptoms had significantly improved, allowing her to rediscover long-lost pleasures like food and music.
This significant progress highlights how DBS has the potential to completely transform the way severe depression is treated.
Despite the positive outlook for DBS, some medical experts advise caution, pointing out possible surgical risks and the need for additional research into the brain mechanisms behind depression.
However, the current studies and clinical trials—including a major one conducted by Abbott Laboratories—indicate that this is a rapidly developing sector that may soon provide people who have not responded to conventional medications fresh hope.
The future of treating depression appears increasingly bright as long as experts keep improving the process and customizing it to each patient’s needs.