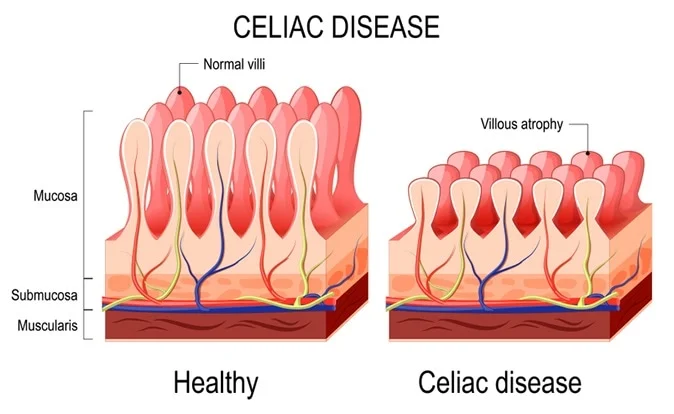
Coeliac disease, also spelled celiac disease, is an autoimmune disorder characterized by an abnormal immune response to gluten, a protein found in wheat, barley, and rye. When individuals with coeliac disease consume gluten, their immune system reacts by damaging the small intestine’s lining, specifically the villi, which are small finger-like protrusions responsible for nutrient absorption. This damage leads to various gastrointestinal and systemic symptoms.
Symptoms:
Symptoms of coeliac can vary widely among individuals and may include:
- Gastrointestinal symptoms: Diarrhea, abdominal pain, bloating, constipation, nausea, vomiting.
- Non-gastrointestinal symptoms: Fatigue, joint pain, anemia, dermatitis herpetiformis (skin rash), osteoporosis, depression, anxiety, and neurological symptoms.
Causes:
The exact cause of the disease is not fully understood, but it is believed to involve a combination of genetic predisposition and environmental factors. Specific genes, such as HLA-DQ2 and HLA-DQ8, are associated with an increased risk of developing coeliac disease. Environmental factors, such as gluten consumption, play a crucial role in triggering the immune response in genetically susceptible individuals.
Prevention:
As coeliac has a strong genetic component, it cannot be entirely prevented. However, early detection through screening of at-risk individuals, such as those with a family history of coeliac disease or certain autoimmune conditions, can lead to early intervention and better management of the condition.
Treatment:
The primary treatment for coeliac is a lifelong strict gluten-free diet. This involves eliminating all sources of gluten from the diet, including wheat, barley, rye, and their derivatives. With adherence to a gluten-free diet, the small intestine typically heals, and symptoms improve or resolve in most individuals.
In addition to dietary modifications, individuals with coeliac disease may require nutritional supplementation to address deficiencies caused by malabsorption. For those with severe symptoms or complications, such as refractory coeliac disease or associated autoimmune conditions, medications and additional medical interventions may be necessary.
Regular follow-up with healthcare providers, including gastroenterologists and dietitians specializing in coeliac disease management, is essential for ongoing monitoring and support.
It’s important for individuals with coeliac disease to be vigilant about reading food labels and identifying hidden sources of gluten, as even small amounts can trigger symptoms and cause intestinal damage. Additionally, maintaining a gluten-free lifestyle may require adjustments in various aspects of daily life, including dining out, traveling, and social gatherings.