Tissue-nonspecific alkaline phosphatase is essential for the hydrolysis of pyrophosphate into inorganic phosphate, a process critical for bone and tooth mineralization. In hypophosphatasia, the deficiency or dysfunction of TNSALP leads to an excess of PPi, which inhibits the formation of hydroxyapatite crystals in the bone matrix and dental enamel. This disruption results in weak and poorly mineralized bones and teeth.
The clinical manifestations of HPP can vary widely depending on the age of onset and the severity of the enzyme deficiency. The disease is traditionally classified into several forms based on age of onset and clinical presentation, including perinatal, infantile, childhood, and adult forms.
Clinical Manifestations
- Perinatal Hypophosphatasia: The perinatal form is the most severe and often presents before or shortly after birth. Infants with this form may exhibit severe skeletal abnormalities, including skeletal deformities, bone fractures, and respiratory distress. Many affected infants may not survive past the first few months of life due to complications related to inadequate lung development and severe bone deformities.
- Infantile Hypophosphatasia: In the infantile form, symptoms generally appear within the first six months of life. Affected infants may experience rickets-like symptoms, including poor growth, skeletal deformities such as bowed legs, and a high risk of fractures. Additionally, dental issues such as early loss of primary teeth and defective tooth enamel are common. Infants with this form may also have delayed motor development and difficulties in feeding.
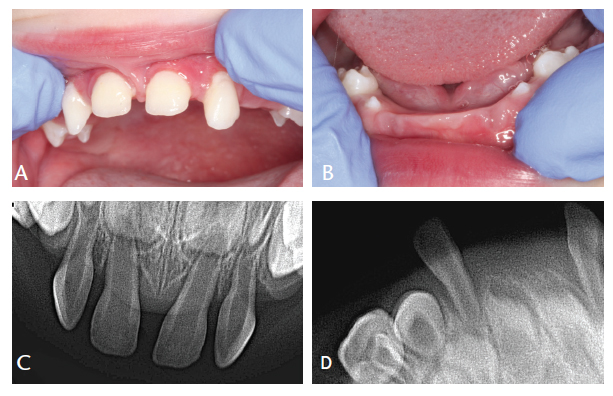
- Childhood Hypophosphatasia: The childhood form typically presents between 6 months and 5 years of age. Symptoms can include growth delays, bone pain, and fractures. Unlike the infantile form, children with this type may not exhibit as severe skeletal deformities but are at risk for developing rickets-like symptoms and dental issues. This form can impact the quality of life due to chronic bone pain and frequent fractures.
- Adult Hypophosphatasia: The adult form of HPP often presents later in life and may be characterized by bone pain, frequent fractures, and premature loss of teeth. Symptoms in adults can be less severe compared to earlier-onset forms but may still significantly affect the individual’s quality of life. Adults with HPP may also experience unexplained bone pain and weakness, which can lead to misdiagnosis or delayed diagnosis.
Diagnosis
Diagnosis of hypophosphatasia is based on a combination of clinical features, biochemical tests, and genetic analysis. A key laboratory finding in HPP is a low serum alkaline phosphatase level. This biochemical marker is often combined with elevated levels of PPi and decreased levels of inorganic phosphate. Imaging studies such as X-rays may reveal characteristic skeletal abnormalities, including osteomalacia, fractures, and deformities.
Genetic testing is essential for confirming the diagnosis and identifying specific mutations in the ALPL gene. This testing can also be useful for family planning and genetic counseling, as HPP is inherited in an autosomal recessive pattern.
Treatment and Management
Currently, there is no cure for hypophosphatasia, and management focuses on alleviating symptoms and improving the quality of life. Treatment strategies may include:
- Enzyme Replacement Therapy (ERT): The approval of asfotase alfa, a recombinant form of TNSALP, has provided a breakthrough in the treatment of HPP. This enzyme replacement therapy aims to address the underlying deficiency by supplementing the deficient enzyme, thereby improving mineralization and reducing symptoms. ERT has shown promise in improving bone mineralization, reducing fractures, and enhancing overall quality of life in affected individuals.
- Supportive Care: Management of HPP often involves a multidisciplinary approach, including orthopedic care, pain management, and physical therapy. Regular monitoring and treatment of skeletal deformities and dental issues are also important components of supportive care.
- Nutritional Support: Ensuring adequate nutritional intake is crucial for individuals with HPP. Although traditional supplementation with calcium and vitamin D may not fully address the mineralization defects, maintaining a balanced diet can support overall health and well-being.
- Genetic Counseling: For families affected by hypophosphatasia, genetic counseling provides valuable information about the inheritance patterns of the disease, implications for future pregnancies, and options for genetic testing.
Prognosis and Future Directions
The prognosis for individuals with hypophosphatasia varies widely depending on the age of onset and the severity of the condition. Advances in research and treatment options, such as enzyme replacement therapy, have significantly improved outcomes for many patients. However, ongoing research is necessary to further understand the disease mechanisms and develop more effective treatments.
In summary, hypophosphatasia is a complex genetic disorder with a broad spectrum of clinical manifestations. Early diagnosis and intervention are crucial for improving outcomes and managing symptoms. As research progresses, there is hope for continued advancements in treatment options, ultimately enhancing the quality of life for individuals affected by this challenging condition.