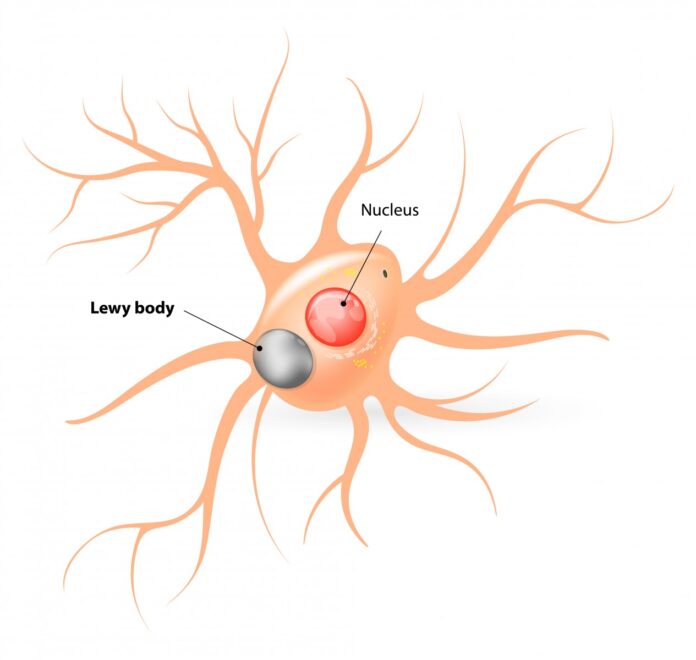
After Alzheimer’s disease, Lewy Body Dementia is the second most prevalent kind of dementia. Brain nerve cells develop protein deposits known as Lewy bodies. The areas of the brain related to thought, memory, and movement are impacted by the protein deposits. Another name for this illness is dementia with Lewy bodies.
Cognitive function declines with Lewy body dementia, becoming worse over time. Individuals suffering from Lewy body dementia may perceive nonexistent objects. We refer to this as visual hallucinations. Additionally, their level of alertness and attention may fluctuate.
It is possible for people with Lewy body dementia to have Parkinson’s disease symptoms. Tremors, slow movement, stiff muscles, and difficulty walking are some of these symptoms.
Symptoms
Symptoms of Lewy body dementia may include:
Visual delusions. Hallucinations, or seeing things that aren’t there, may be one of the initial signs of Lewy body dementia. This symptom is frequently ongoing. Individuals suffering from Lewy body dementia may perceive phantom objects, animals, or persons. It’s possible to experience touch, smell, or sound hallucinations.
Disorders of movement. Parkinson’s disease symptoms, sometimes referred to as parkinsonian signs, can appear. Slower movement, stiff muscles, tremor, or a shuffling gait are some of these symptoms. The person may fall as a result of this.
Inadequate control over bodily processes. The autonomic nervous system is the portion of the nervous system that regulates autonomic processes. The autonomic nervous system’s ability to regulate blood pressure, heart rate, perspiration, and digestion can be impacted by lewy body dementia. This may cause abrupt drops in blood pressure when standing, vertigo, falls, loss of control over one’s bladder, and digestive problems like constipation.
Mental issues. Cognitive impairments associated with Lewy body dementia may resemble those of Alzheimer’s disease. Confusion, inattention, visual-spatial issues, and memory loss are a few of them.
Issues with resting. Sleep behaviour disorder characterised by rapid eye movement (REM) can occur in people with Lewy body dementia. People with this disorder act out their dreams while they are asleep. When they’re asleep, people with REM sleep behaviour disorder may kick, punch, shout, or scream.
Shifting the focus. It’s possible to experience periods of sleepiness, extended periods of staring into space, prolonged naps during the day, or rambling speech.
Depression. Depression is possible in people with Lewy body dementia.
Lack of interest. Motivation may fade away.
Causes
Lewy bodies, which are protein accumulations in the brain, are indicative of Lewy body dementia. Parkinson’s disease is also linked to this protein. Alzheimer’s disease plaques and tangles are also present in people with Lewy bodies in their brains.
Treatment
DLB has no known cure. Treatments may enhance your quality of life and assist in managing symptoms.
Drugs
Drugs can lessen or manage symptoms that impact your mood, movement, sleep, and cognitive function. These drugs could consist of:
Cholinesterase inhibitors: Drugs like galantamine, rivastigmine, and donepezil raise brain levels of neurotransmitters essential for cognition, alertness, and memory. They lessen the cognitive issues that some DLB sufferers face.
Antidepressants: Depression and mood swings are treated with drugs like selective serotonin reuptake inhibitors (SSRIs).
Carbidopa-levodopa: This medication functions by raising dopamine levels in the brain. Slower movements, stiffness, or tremors are some of the Parkinson’s-like symptoms that it may help lessen in DLB patients.
Melatonin and clonazepam are two drugs that treat REM sleep behaviour disorder to enhance the quality of sleep.
Memantine: This drug lowers the brain’s glutamate chemical messenger. Particularly, moderate-to-severe dementia is treated with it.
Pimavanserin: People with Parkinson’s disease dementia who experience hallucinations and delusions are treated with this medication. It might be beneficial for DLB sufferers who experience these symptoms.
Therapeutic Interventions for Rehabilitation
Rehabilitative therapies can lessen complications, control symptoms, and enhance your quality of life. Your neurologist might suggest:
Occupational therapy: Occupational therapists can assist you in discovering fresh approaches to carrying out routine tasks.
Physical therapy: Exercises to increase balance, lower the risk of falls, and maintain an active lifestyle are taught by physical therapists.
Psychotherapy: Psychotherapists can assist you in controlling the melancholy and anxiety that frequently accompany DLB. They might recommend anxiety or depression medications.
Speech therapy: A speech therapist can help you swallow and eat more efficiently as well as communicate more clearly.